Share this post!
Fiber, Microbiota, and Mucus are Essential for Colon Health
At first, it may seem that these ingredients – fiber, bacteria, and mucus – are unlikely to work together, let alone provide an important recipe for robust intestinal function. But when you look closely at the relationships between these factors, it’s hard to deny how important they are to digestive health.
Fiber is one of those nutrients whose benefits to humans are relatively widely known and accepted. However, the mechanisms of its action, especially through its interaction with microbiota, are less understood. New research is coming out every day on the importance of the microbiome for health, furthering our scientific understanding of the trillions of tiny friends that live with our bodies.
In this article, we’ll define fiber and its varieties, describe its importance to microbiota, discuss mucus and its relevance in the gastrointestinal tract, and highlight the significance of this trio in maintaining health of the colon.

Fiber
Dietary fiber is a complex carbohydrate that our body is not equipped to digest. It comes in many forms, the simplest distinction being whether the fiber is soluble, or absorbed in the body, or insoluble, not absorbed in the body. All of these carbohydrates qualify as a type of fiber:
- Non-starch polysaccharides, or many (>10) sugar molecules bonded together
- Celluloses
- Hemicelluloses (such as the fibers found in cranberries)
- Pectins
- Hydrocolloids
- Fructo-oligosaccharides
- Resistant starches
Within these categories are numerous variations in chain length, types of simple sugar, and bond locations, which result in a vast diversity of fibers.
Benefits of dietary fiber include improved gut motility (i.e. the movements of the digestive system and transit of its contents), increased insulin sensitivity, and reduction of inflammation with effects on mood and cardiovascular function.
Unlike simple sugars and starches, the human body cannot digest fiber because it lacks the necessary enzymes to break the bonds in these large, complex molecules. However, there are organisms that can.
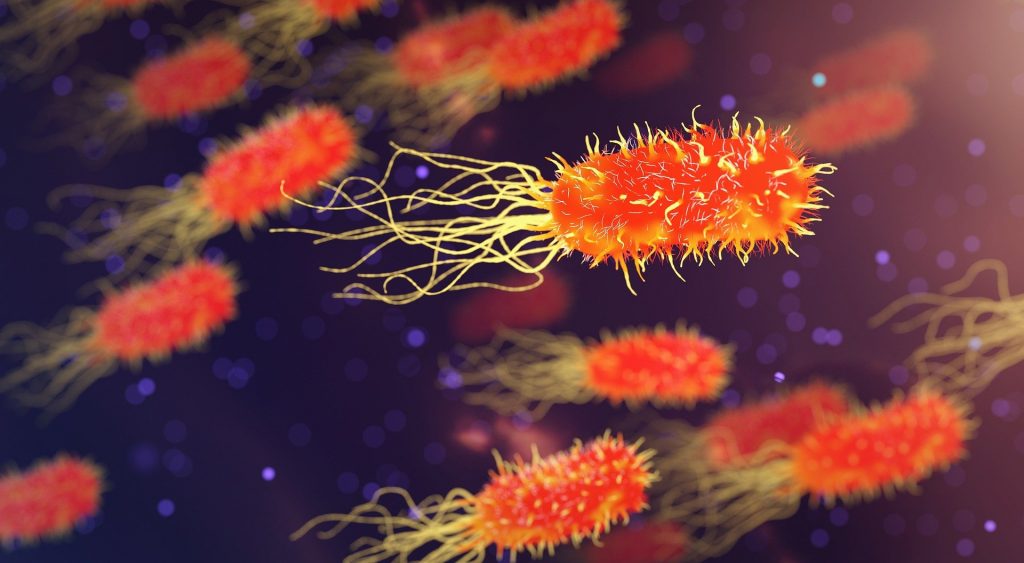
Microbiota
The human digestive system only makes about 17 enzymes to help break down foods into the simple sugars and amino acids used in metabolism. Luckily, trillions of tiny microorganisms evolved with us to fill in the gaps. These tiny microorganisms are collectively referred to as the microbiome, and their vast diversity of species accounts for the many additional enzymes they produce that help us digest complex carbohydrates and other nutrients.
Bacteria in our digestive tract, particularly those in the colon, make enzymes that break down the polysaccharides into smaller fragments and simple sugars. Microbiota then anaerobically (i.e. without oxygen) ferment these smaller fragments, resulting in the production of short-chain fatty acids (SCFAs).
SCFAs provide a huge benefit to the host, primarily as an energy source for colonocytes (cells of the colon), but they also have significant roles in regulating various aspects of metabolism and brain function. One particular function of SCFAs is to enhance mucus production, a crucial aspect of colon health.
Mucus
Mucus’s main role is to protect the cells of the digestive system from infection and damage. It also keeps the GI tract lubricated for its contents to move along smoothly. In the colon, there are two layers of mucus – the inner layer and the outer layer.
The inner layer of mucus is attached to the epithelial wall of the colon, or the gut lining. This layer is designed to protect the single celled layer that separates the body from its external environment, therefore it is dense and keeps bacteria out. In contrast, the outer layer is less dense, not attached, and colonized by trillions of bacteria.
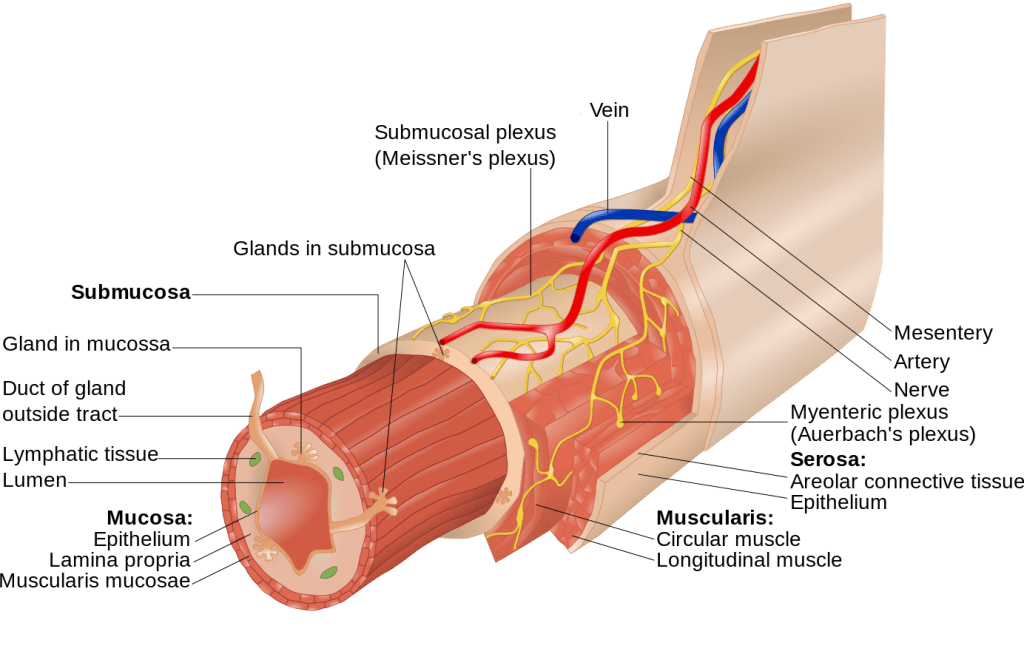
There are many types of mucus, but the main variety at play in the colon is MUC2, a gel-forming mucus. At the core of mucus particles is a cluster of amino acids – typically proline, serine, and threonine – that bond together in a rod-like formation. These protein clusters, known as domains, are covered in glycans (another word for polysaccharides) that protect the protein core from digestion by proteases (protein-digesting enzymes) in the GI tract. The composition of this type of mucus is about 80% glycans and 20% protein, with the glycan portion being able to absorb a considerable amount of water giving the mucus a gel-like consistency.
Recall that microbiota’s favorite food is complex polysaccharides, like fiber. But what happens if their meal never shows up?
Microbiota Use Mucus as a Food Source
In the event of inadequate dietary fiber, microbiota resort to digesting the polysaccharide component of mucus. This compromises the integrity of the mucosal layer by altering bacterial populations and thinning mucus, as shown by this 2016 study.
The researchers colonized mice with human gut bacteria, then fed them either fiber-rich diets, fiber-free diets, or a prebiotic diet (which included purified fibers such as inulin or β-glucan). In order to mimic typical dietary patterns that naturally vary in fiber, some mice were fed a diet that rotated from fiber-rich to fiber-free to measure the effect of intermittent fiber deficiency.
Results from the study showed that the lower fiber diets altered microbial populations to favor species that were able to degrade the mucus and use it as a food source. Even the intermittently fiber-deprived diets showed this effect, as well as a notable shift in populations based on whether fiber was present or not as measured by changes in gene expression and enzyme readouts.
When measuring mucosal thickness, the fiber-rich diets in the colonized mice had the most robust layer of mucus. Thinner mucus was noted in the fiber-free, prebiotic, alternating groups, as well as the germ-free (no microbiota) control group, which suggests microbial involvement in the generation of mucus.
Interestingly, the prebiotic diet, containing purified soluble fibers like those found in prebiotic supplements, was not able to restore mucosal thickness, although these isolated fibers did alter bacterial populations, suggesting that perhaps naturally occurring fiber is more than the sum of its parts.
Furthermore, the authors show that dietary fiber insufficiency also leaves the colon more susceptible to pathogenic infection and subsequent inflammatory response.
Fiber and the Reduction of Inflammation
In the GI tract, mucus is the first layer of defense against bacteria. Thinner mucosal layers allow potential pathogenic bacteria to be closer to the surface of human cells. In addition, mucus contains antimicrobial and immunoglobulins to help neutralize pathogens before they elicit an inflammatory response.
Butyrate, a short-chain fatty acid produced by gut bacteria, is anti-inflammatory, can improve oxidative stress within the colon, and protects the intestinal barrier to prevent leakiness, in addition to providing energy for colonocytes.
Clinical Application
Diverticula are bulges or sacs that occur in the digestive tract, particularly in the colon. They are fairly common, especially in older populations, where as many as 70% of people over age 70 have them. Diverticulosis is simply the presence of diverticula. Diverticulitis occurs when diverticula become infected.
Since the 1960s, the theory has been that a low-fiber diet is a causative factor in the development of diverticulosis, though research has never proven that claim. Though high-fiber diets may not prevent the onset of diverticulosis, they have been shown to decrease the risk of developing diverticulitis. The mechanism of this protection may be related to the health benefits of fiber intake on the microbiome and mucus production that protect the colon from pathogenic infection.

Sources of Fiber
Fruits, vegetables, whole grains, legumes, nuts and seeds are all great sources of fiber. It is important to obtain fiber from a variety of sources, as fruits and vegetables tend to be more concentrated in soluble forms of fiber, while grains and legumes contain more insoluble fibers. These foods in their natural state will contain a mixture of soluble and insoluble fibers, mimicking the natural fibers found in the fiber-rich diets of the research model that resulted in increased mucosal thickness and optimal microbial populations.
Tying it all Together
Ample dietary fiber provides nutrients to sustain thriving beneficial microbiota so they may generate SCFAs and produce and maintain a robust layer of mucus for a happy and healthy gastrointestinal tract.
Related reading…
Enhancing Gut Health: The Power of Prebiotics
Understanding Probiotics and Prebiotics
About the author: Karyn Lane is a current student of NTI’s Nutrition Therapist Master Program. She finds her chemistry degree a useful tool in her study of nutrition and loves to treat herself as a laboratory for new recipes and cooking techniques. You can follow her on Instagram @feel.alive.nourishment.
Learn more about our school by attending an informational webinar.
Images: Image by Maksim Shutov is free for use by Unsplash; Image by Dan Gold is free for use by Unsplash; Image by kimono is free for use by Pixabay; Image by Goran tek-en is licensed under CC BY-SA 3.0; Image by Jannis Brandt is free for use by Unsplash
Share this post!